Breathe Easier, Live Easier
Always feel short of breath? We retrain how you breathe, here in Ottawa.
“In the Buteyko group the proportion with asthma control increased from 40% to 79%.”
- Cowie RL, Conley DP, Underwood MF, Reader PG
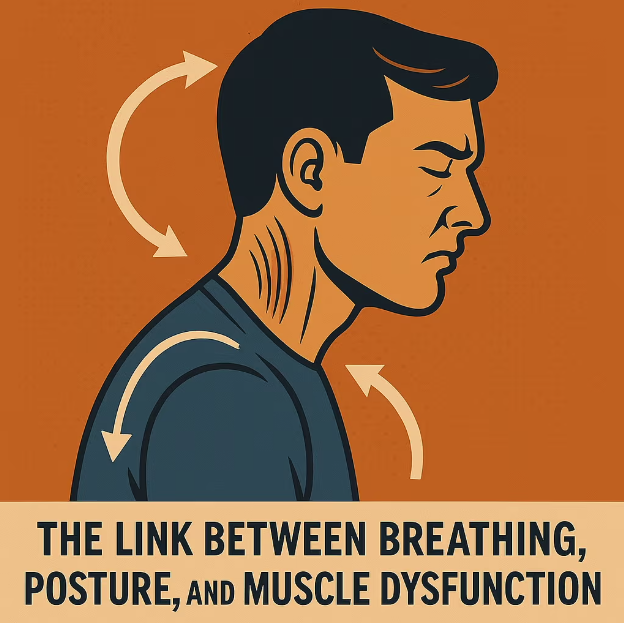
The Pattern
Many people overbreathe - too fast, too high in the chest - causing air hunger even at rest.
The Skill
We teach nasal, diaphragmatic breathing, + open the airway, to calm the body and make breathing feel easier.

The Plan
Short daily micro-routines (2-5 min) + biweekly coaching.
Safe, practical, measurable.
Is This You?
Can’t get a deep breath unless you sigh or yawn
Mouth breathing and a dry throat, day or night
Breathing lives in the upper chest/neck
Winded by stairs, conversations, or mild stress
Faster breathing at rest or frequent overbreathing
Waking unrefreshed; dry mouth in the morning
*If you have chest pain, wheeze, fainting, or blue lips/fingers, seek urgent care first.
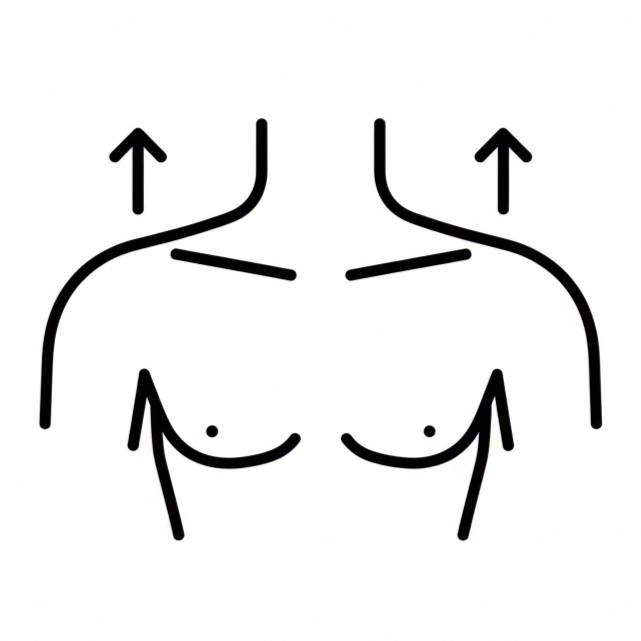
Chest vs. Diaphragmatic Breathing
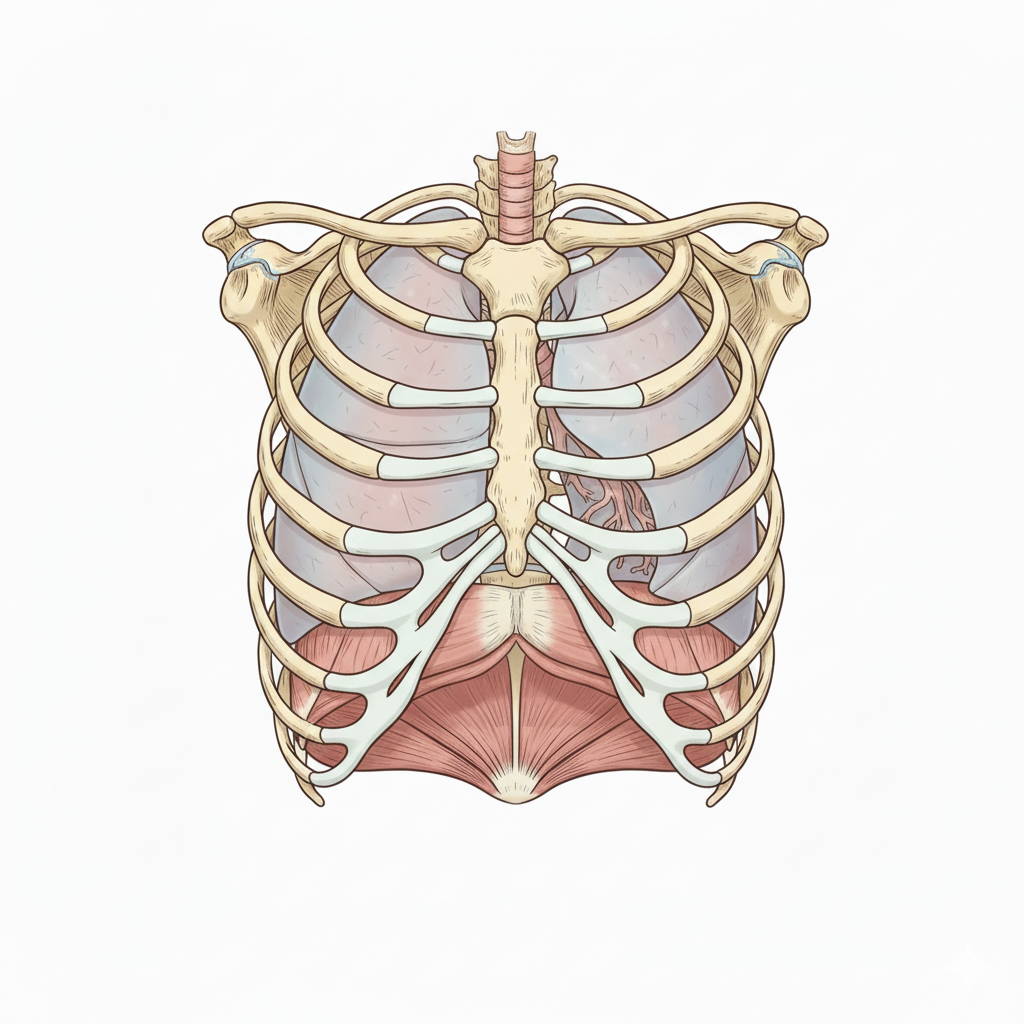
Chest
Fast, shallow, shoulders lift
Accessory muscles overworked
Chronic hyperventilation - low CO₂ - air hunger
Feeds fight-or-flight; tension, anxiety
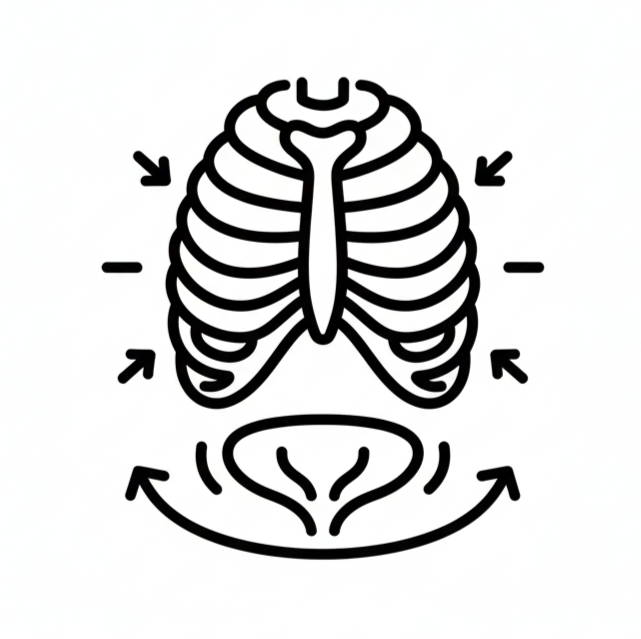
Diaphragm
Quiet, slow, light, nasal
Lower ribs expand gently
Better CO₂ balance - calmer breath, increased O₂ intake
Easier energy throughout the day
60-Second Self-Check

Sit tall. One hand on upper chest, one on your belly.
Breathe quietly through your nose for 6–10 breaths.
If the top hand lifts first/most → chest-dominant.
If the lower hand widens gently → diaphragm engaged.
What We Do
Nasal Breathing Skills
Goal: Decongest the nose, clear sinuses, open the airway, tone the lips.
How: Gentle nasal prep, lip-seal cues, light/quiet breathing.
Diaphragm Mechanics
Goal: Low-rib expansion; build tone and flexibility in the diaphragm; soften neck/jaw.
How: Graduated breathing exercises so the lower ribs begin to expand 360° while shoulders stay relaxed.
Overbreathing Reduction
Goal: Rebuild CO₂ tolerance, reduce air hunger, support steadier oxygen delivery.
How: Slow, light nasal breathing by day and night; smaller, calmer breaths.
Oral Posture
Goal: Tongue-to-palate, lip seal, calm jaw support.
How: Rest tongue gently suctioned on the palate, lips lightly together, teeth slightly apart; breathe through the nose.
Sleep-Aware Habits
Goal: Support an open airway and calmer breathing overnight.
How: Evening nasal prep, night airway therapy; coordination with your dentist/MD as needed.
Try This
Inhale so just your lower (belly) hand expands; keeping the chest hand still. Practice this through the day.
Struggling With This
Breathing Benefits of Orofacial Myofunctional Therapy

Nasal nitric oxide (NO)
Nasal breathing naturally releases small amounts of NO. It helps airways stay open, supports blood flow, and adds mild antimicrobial defense in the nose.
Better oxygen use throughout the body
Calmer, slower nasal breathing improves the way oxygen is delivered to your tissues, so you feel less winded during everyday tasks.
Bohr effect
When you stop “chasing air” and allow healthy CO₂ levels, your blood lets go of oxygen more easily to the muscles and brain.
Deeper, calmer diaphragmatic breaths
Low-rib expansion gives those deep, satisfying breaths without shoulder/neck strain.
Calmer nervous system (Vagus support)
Quiet, nasal breathing helps down-shift fight-or-flight and encourages a steadier, relaxed state.
Better, more refreshing sleep
More nasal breathing and less mouth breathing reduce dryness and night wakings; you wake feeling more rested.
More steady energy
Fewer breath spikes and less air hunger mean smoother energy through the day.
Less upper-back and neck tension
Breathing with the diaphragm lets the accessory muscles (SCM, scalenes, upper traps) relax.
Jaw comfort
Tongue-to-palate posture and lip seal support a more open nasal airway and calmer jaw muscles, easing clenching, overworked patterns.
Your Myofunctional Therapy Breathing Plan
Simple daily skills. Real-life results.

01. Free Consultation
We listen to your symptoms and concerns and explain how breathing retraining works. You’ll learn what we do and whether it fits your goals. Clear next steps, no pressure.

02. Assessment & Baseline Exam
A detailed look at your breathing pattern: oral posture, lip toning, airway, congestion, and muscle imbalances. We take thorough measurements to map disorders and identify where your specific breathing difficulties stem from.

03. Diagnosis & Tailored Treatment Plan
We put your findings into a clear picture: what’s happening, why it feels that way, and how we can help. Your plan is tailored to your needs and abilities, including simple micro-routines, frequency, and how we’ll measure progress.

04. Coaching & Progress
Step-by-step exercises you can do daily (2–5 minutes at a time). You’ll see results build—breathing feels easier, energy steadier, and the neck/chest strain fades. We review, fine-tune, and expand skills as you improve.
What Is Orofacial Myofunctional Therapy?

Orofacial Myofunctional Therapy is focused “muscle and habit” training for the tongue, lips, jaw, and airway. We teach nasal, diaphragm-led breathing and healthy oral posture (tongue to palate, lips closed, jaw relaxed) so breathing feels calmer and more efficient—day and night. This reduces mouth breathing, chest-dominant overbreathing, frequent sighing/yawning, and that “can’t get a full breath” feeling, while easing neck/throat tightness.
Therapy starts with a detailed breathing-focused assessment (posture, nose vs. mouth use, rib movement), then simple targeted exercises and micro-routines that you weave into daily life—during rest, conversations, light activity, and sleep. By restoring low-rib expansion and airway-supportive tongue posture, you build steadier CO₂ tolerance, smoother nasal airflow, and a quieter rhythm—so you feel less winded and more at ease.
Frequently asked questions
Why am I short of breath if medical tests are normal?
Do you use Buteyko breathing techniques?
Do I have to tape my mouth?
How soon will I feel a difference?
I have allergies and/or asthma—can you still help?
What age can we start?
When should I see a doctor first?
Ottawa, Ontario Clinic
1193 St. Laurent Blvd
Inside the East Ottawa Dental Clinic
Monday, 8am to 4pm
Tuesday & Wednesday, 10am to 6pm
Thursday to Saturday, 9am to 5pm
Sunday, Closed
You are in advanced mode.
You can turn it off in left sidebar. To use advanced options, you will need to enter your own Google Maps API Key.
Get Google API KeyBy Jan 04, 2026
By Oct 12, 2025
By Oct 01, 2025
By Aug 10, 2025
By Jul 10, 2025
By Jul 05, 2025