Adult Facial Pain Relief in Ottawa – Therapy for Jaw Tension, Muscle Strain, and TMJ Symptoms
Struggling with facial tension, aching jaws, or unexplained pain in your cheeks, temples, or neck? We address the muscular root of your symptoms—without medication or invasive treatment.
Your head, neck, face, & mouth are in a complex delicate balance.
Any small "normal habit" can throw this incredible system out of whack causing discomfort.
The Advantage Program helps you find your new oral-facial balance
with simple scientifically designed exercises for long lasting benefits.
The Advantage Program Designs Your Program to Your Needs
These Are The Many Causes Of Facial Pain
Unhealthy Breathing Pattern
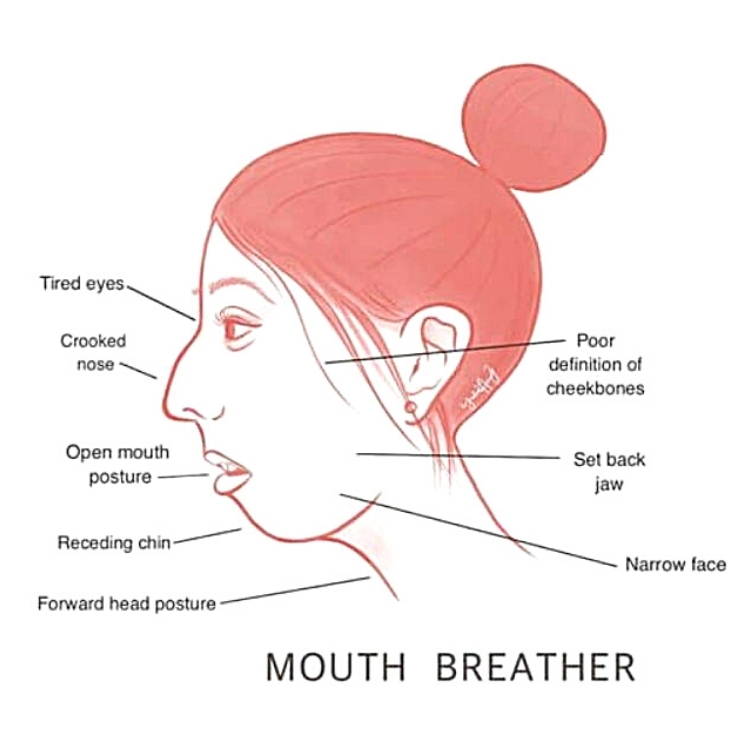
Mouth Breathing
Mouth Breathing Can Cause Restrictions in the Airway21,20,23
Causes Long Face Syndrome11,16,19,23
Crooked Teeth
Narrow Jaw and Face
Poorly Defined Cheekbones
Tired Eyes
Jaw Set Back
Smaller Airway
Underdeveloped Nasal Airway
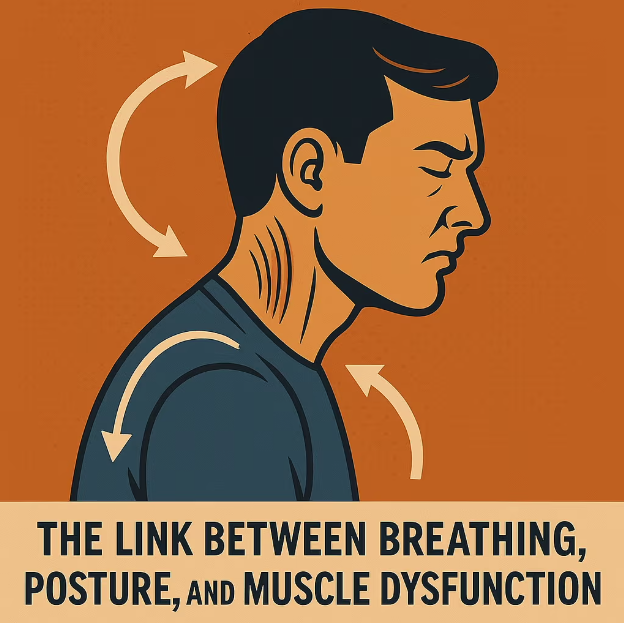
Postural Problems: Mouth breathers tend to assume a characteristic posture, carrying their heads forward in order to compensate for the restriction to their airways and make breathing possible.20
The forward head posture often leads to: muscle fatigue, neck pain, tension in the TMJ area, spinal disc compression, early arthritis, tension headaches, and dental occlusal problems.21

Upper Chest Breathing
We are designed to use our diaphragm to breathe. Breathing with our upper chest puts strain on our backs and necks which can cause pain39
Can contribute to stress, anxiety, brain fog, and poor body oxygenation24
Causes shorter shallower breaths, which is directly related to increasing blood pressure24
Gas exchange is hindered: the entire lung is not used when upper chest breathing, preventing efficient gas exchange.24 Poor oxygenation can cause:35
Nervous System: Feeling faint, headache, migraine, numbness or pins and needles, difficulty tolerating light, dizziness and unsteadiness
Muscular: Cramps, muscle pains, stiffness, tremors
General: Weakness, fatigue, poor concentration, impaired memory and performance, sleep disorders, night sweats, brain fog, allergies
Sleep Disordered Breathing
Places the jaw in muscle and tissue stressing positions21
Prevents deep sleep which can cause headaches/migraines12 and prevent the release of Growth Hormone31,32,33
Causes dehydration which puts stress on the muscles and tissues22,46
Negatively affects oxygen levels which strains the cardiovascular system4,12,24,35
An open mouth can cause sleep disordered breathing even if breathing through the nose. The soft palate, when the mouth is open, can block the nasal breathing passageway12


Damaging Oral Resting Postures
Tongue Settles in Atypical Area of the Mouth
Incorrect Tongue Resting Posture: Can cause the palate to narrow and vault, crowding the teeth and making the nasal cavity smaller17,18,19
The tongue from the tip to the posterior needs to be toned to rest in the palate. Most tongues are untrained/untoned, which can cause snoring and apnea.35,36
The tongue, even when untoned, is still 8 strong muscles. Resting incorrectly puts a lot of pressure against oral structures that don't have the strength to resist.17,18,19
Ankyloglossia (tongue-tied): A condition where the tongue has a varying degree of restriction (a reduced range of motion) causes the muscles, and tissues in the head and neck region to over-compensate. This has many side-effects.25,26,27,28,29,30
Incorrect Swallow Pattern
Tongue Thrust17,18,19
Bone Loss Around Specific Teeth17,18
Tooth Mobility17,18
Open Bites & Malocclusion17,18


Daily Repetitive Habit Involving Your Mouth
Thumb/Finger/Lip Sucking, Nail, Cheek, Tongue, Hair, or Object Chewing...etc.
When we consistently place something in the way of the teeth and oral structures, the anatomy will slowly form around this obstruction. Like a tree will form around a fence that is in its growth path36,37,38,39,41
Can cause vaulted palates narrowing therefore shrinking the nasal canal and sinuses causing nasal congestion.37,38
Open bites, narrow jaw, long face syndrome, asymmetrical face36,37,38,39,41
Can cause sleep disordered breathing12
Putting the jaw in a repetitive incorrect position can cause severe muscle/tissue/joint strain19
Book a Free In-Person Consultation Today

Benefits of Orofacial Myofunctional Therapy
Soothes some headaches
Can help reduce snoring & apnea
Opens upper airways
Eases long face syndrome
Alleviates facial pain
Improves posture & core muscle stability
Increases jaw range of motion
Tones facial muscles & tissues
Improves focus & memory
Lowers harmful stress hormones
Relieves digestive discomfort
Plus much more
What is Orofacial Myofunctional Therapy?
The mouth, head, and neck are a complex weave of muscles, tissues, joints, bones, blood vessels, and nerves that all need to work together for a smooth, discomfort-free daily function.
We are born and grow with little direction and training in this area of our bodies. We eat the way we eat, we chew on the side that is most comfortable, we swallow whichever way gets the food down, our tongues rest wherever they rest, we breathe the easier way, and we have repetitive habits that soothe our stress that can involve our faces and mouths.
All of these reflexive habits can create abnormalities in our oral and facial structures, and since we have been doing them throughout youthful growth, our bones and muscles have molded around these untrained habits, potentially creating ingrained disorders in our current and later years.
Orofacial Myofunctional Therapists specialize and only focus on the muscles and tissues throughout the tongue, jaw, face, head, and neck. Weekly exercises are given that either tone or relax these muscles and tissues aligning them to your center. Working from your foundation up, we progressively reset years of habits. Most individuals will complete the program within the year and yet your new symmetry could last your lifetime.
A Stanford University Systematic Review Revealed The Lasting Beneficial Effects Of Orofacial Myofunctional Therapy In A Wide Cohort:
“Current literature demonstrates that orofacial myofunctional therapy decreases apnea-hypopnea index by approximately 50% in adults and 62% in children. Improvements to snoring and daytime sleepiness. Shown effective in children and adults of all ages studied thus far; youngest patient 3 yrs old to 60 yrs old. Therapy has an important role in preventing relapse.”48
1Key, Josephine. “‘The core’: understanding it, and retraining its dysfunction.” Journal of bodywork and movement therapies 17, no. 4 (2013): 541-559.
2Gunduz C, et al "Obstructive sleep apnea independently predicts lipid levels: Data from the European Sleep Apnea Database" Respirology 2018; DOI: 10.1111/resp.13372.
3Jimmy Doumit, Bharati Prasad. "Sleep Apnea in Type 2 Diabetes" Diabetes Spectrum 2016 Feb; 29(1): 14-19.
4Omar A. Mesarwi, Rohit Loomba, Aul Malhotra. "Obstructive Sleep Apnea, Hypoxia, and Nonalcoholic Fatty Liver Disease" ATS Journals 2018 Nov; V199, I7.
5Bharati Prasad, Sharmilee M. Nyenhuis, Ikuyo Imayama. "Asthma and Obstructive Sleep Apnea Overlap: What has the evidence taught us?" ATS Journals 2019 Dec;V201, I11.
6Ejaz, Shakir M et al. “Obstructive sleep apnea and depression: a review.” Innovations in clinical neuroscience vol. 8,8 (2011): 17-25.
7Djupesland PG, Chatkin JM, Qian W, Haight JS. Nitric oxide in the nasal airway: a new dimension in otorhinolaryngology. Am J Otolaryngol.2001 Jan; 22(1): 19-32.
8Lunn M, Craig T. Rhinitis and sleep. Sleep Med Rev. 2011 Oct;15(5):293-9
9Muliol J, Maurer M, Bousquet J. Sleep and allergic rhinitis. Journal Investigation Allergol Clinical Immunology. 2008;18(6):415-9.
10Ohki M, Usui N, Kanazawa H, Hara I, Kawano K. Relationship between oral breathing and nasal obstruction in patients with obstructive sleep apnoea. Acta Otolaryngol Suppl. 1996;523:228-30.
11Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics and behaviour. General dentist. 2010 Jan- Feb; 58 (1): 18-25.
12Fitzpatrick MF, McLean H, Urton AM, Tan A, O’Donnell D, Driver HS. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J. 2003 Nov;22(5):827-32.
13“ADHD and Sleep.” ADHD & Sleep Problems-National Sleep Foundation. National Sleep Foundation, 2017. Web. 11 Feb.2017. https://sleepfoundation.org/sleep-disorders-problems/adhd-and-sleep.
14Shur-Fen Gau S. Prevalence of sleep problems and their association with inattention/hyperactivity among children aged 6-15 in Taiwan.J Sleep Res. 2006 Dec;15(4):403-14.
15Borres MP. Allergic rhinitis: more than just a stuffy nose. Acta Paediatrica. 2009 Jul;98(7):1088-92)
16Pereira F, Motonaga S, Faria P, Matsumoto M, Trawitzki L, Lima S, Lima W. Myofunctional and Cephalometric Evaluation of Mouth Breathers. Brazilian Journal of Otorhinolaryngology. 2001. 67 (1): 43-49.
17Garliner D. Myofunctional Therapy. Philadelphia: Saunders, 1976. Print.(10-12)
18John E. Hall, Arthur C Guyton. Tongue posture and swallowing. Guyton and Hall textbook of medical physiology, 12th edition. 2010; 763-765.
19Paskay L. OMD Orofacial Myofunctional Disorders: Assessment, prevention and treatment. JAOS. 2012 march-april; 34-40.
20Okuro RT, Morcillo AM, Ribeiro MÂ, Sakano E, Conti PB, Ribeiro JD. Mouth breathing and forward head posture: effects on respiratory biomechanics and exercise capacity in children. J Bras Pneumol.2011 Jul-Aug; 37(4):471-9.
21Damaging Effects of Forward Head Posture.(2015, January 22). Retrieved from http://www.denvertechchiro.com/files/fhp_revised.pdf
22Svensson S, Olin AC, Hellgren J. Increased net water loss by oral compared to nasal expiration in healthy subjects. Rhinology. 2006 Mar;44(1):74-7. PMID: 16550955.
23Surtel A, Klepacz R, Wysokińska-Miszczuk J. Wpływ toru oddechowego na jamę ustną [The influence of breathing mode on the oral cavity]. Pol Merkur Lekarski. 2015 Dec;39(234):405-7. Polish. PMID: 26802697.
24Steffen, Patrick R et al. “The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood.” Frontiers in public health vol. 5 222. 25 Aug. 2017, doi:10.3389/fpubh.2017.00222
25Tongue-tie (ankyloglossia). American Academy of Otolaryngology-Head and Neck Surgery. http://www.entnet.org/content/tongue-tie-ankyloglossia. Accessed Feb. 13, 2018.
26Isaacson GC. Ankyloglossia (tongue-tie) in infants and children. https://www.uptodate.com/contents/search. Accessed Feb. 14, 2018.
27Chinnadurai S, et al. Treatment of ankyloglossia for reasons other than breastfeeding: A systemic review. Pediatrics. 2015;135:e1467.
28Baker AR, et al. Surgical treatment of ankyloglossia. Operative Techniques in Otolaryngology. 2015;26:28.
29Walsh J, et al. Diagnosis and treatment of ankyloglossia in newborns and infants. JAMA Otolaryngology-Head and Neck Surgery. 2017;143:1032.
30O'Shea JE, et al. Frenotomy for tongue-tie in newborn infants. Cochrane Database of Systemic Reviews. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD011065.pub2/abstract. Accessed Feb. 14, 2018.
31Davidson, J R et al. “Growth hormone and cortisol secretion in relation to sleep and wakefulness.” Journal of psychiatry & neuroscience : JPN vol. 16,2 (1991): 96-102.
32Takahashi, Y et al. “Growth hormone secretion during sleep.” The Journal of clinical investigation vol. 47,9 (1968): 2079-90. doi:10.1172/JCI105893
33Honda, Y et al. “Growth hormone secretion during nocturnal sleep in normal subjects.” The Journal of clinical endocrinology and metabolism vol. 29,1 (1969): 20-9. doi:10.1210/jcem-29-1-20
34Morabito G, et al. (2014). Functional aerophagia in children: A frequent, atypical disorder. DOI:10.1159/000362441
35Timmons, Beverly H., and Ronald Ley. “Behavioral and Psychological Approaches to Breathing.
36https://news.stanford.edu/2020/07/21/toll-shrinking-jaws-human-health/
37Schmidt JE, Carlson CR, Usery AR, Quevedo AS. Effects of tongue position on mandibular muscle activity and heart rate function. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:881-888
38Warren JJ, Slayton RL, Bishara SE, Levy SM, Yonezu T, Kanellis MJ. Effects of nonnutritive sucking habits on occlusal characteristics in the mixed dentition. Pediatr Dent. 2005 Nov-Dec;27(6):445-50. PMID: 16532883.
39Bishara SE, Warren JJ, Broffitt B, Levy SM. Changes in the prevalence of nonnutritive sucking patterns in the first 8 years of life. Am J Orthod Dentofacial Orthop. 2006 Jul;130(1):31-6. doi: 10.1016/j.ajodo.2004.11.033. PMI: 16849069.
40Farsi NM, Salama FS. Sucking habits in Saudi children: prevalence, contributing factors and effects on the primary dentition. Pediatr Dent. 1997 Jan-Feb;19(1):28-33. PMID: 9048410.
41Garattini G, Crozzoli P, Valsasina A. Ruolo del succhiamento protratto nell'insorgenza di alterazioni dento-scheletriche del distretto facciale: revisione della letteratura [Role of prolonged sucking in the development of dento-skeletal changes in the face. Review of the literature]. Mondo Ortod. 1990 Sep-Oct;15(5):539-50. Italian. PMID: 2280788.
42Kuijpers-Jagtman AM. Gevolgen van zuiggewoonten voor de ontwikkeling van het tandkaakstelsel [Effects of sucking habits on the dentofacial development]. Ned Tijdschr Tandheelkd. 1989 Jun;96(6):256-8. Dutch. PMID: 2635279.
43Estripeaut LE, Henriques JF, de Almeida RR. Hábito de sucção do polegar e má oclusão--apresentação de um caso clínico [Thumbsucking and malocclusion--presentation of a clinical case]. Rev Odontol Univ Sao Paulo. 1989 Apr-Jun;3(2):371-6. Portuguese. PMID: 2639459.
44Grippaudo C, Paolantonio EG, Antonini G, Saulle R, La Torre G, Deli R. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngol Ital. 2016 Oct;36(5):386-394. doi: 10.14639/0392-100X-770. PMID: 27958599; PMCID: PMC5225794.
45Doğramacı EJ, Rossi-Fedele G. Establishing the association between nonnutritive sucking behavior and malocclusions: A systematic review and meta-analysis. J Am Dent Assoc. 2016 Dec;147(12):926-934.e6. doi: 10.1016/j.adaj.2016.08.018. Epub 2016 Sep 28. PMID: 27692622.
46Lee SH, et al. How Does Open-Mouth Breathing Influence Upper Airway Anatomy? The Laryngoscope 2007; 117:1102-1106. https://doi.org/10.1097/MLG.0b013e318042aef7
47Meerman R, Brown A J. When somebody loses weight, where does the fat go? BMJ 2014; 349 :g7257 doi:10.1136/bmj.g7257
48Camacho, Macario et al. “Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review and Meta-analysis.” Sleep vol. 38,5 669-75. 1 May. 2015, doi:10.5665/sleep.4652
49Merck Manual Professional Version. Gas-related complaints. https://www.merckmanuals.com/professional/gastrointestinal-disorders/symptoms-of-gi-disorders/gas-related-complaints?query=gas-related complaints#. Accessed Jan. 8, 2020.
50Chitkara DK, Bredenoord AJ, Rucker MJ, Talley NJ. Aerophagia in adults: a comparison with functional dyspepsia. Aliment Pharmacol Ther. 2005 Nov 1;22(9):855-8. doi: 10.1111/j.1365-2036.2005.02651.x. PMID: 16225495.
51Abraczinskas D. Overview of intestinal gas and bloating. https://www.uptodate.com/contents/search. Accessed Jan. 8, 2020.
52https://www.healthline.com/health/aerophagia
53Proffit WR. Contemporary Orthodontics Fourth Edition. Elsevier, Health Sciences Education, Marketing.
54Guimarães KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filho G. "Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome." Am J Respir Crit Care Med. 2009 May 15;179(10):962-6. doi: 10.1164/rccm.200806-981OC. Epub 2009 Feb 20. PMID: 19234106.
55de Felício, Cláudia Maria et al. “Obstructive sleep apnea: focus on myofunctional therapy.” Nature and science of sleep vol. 10 271-286. 6 Sep. 2018, doi:10.2147/NSS.S141132
56Trevisan, Maria Elaine, Jalusa Boufleur, Juliana Corrêa Soares, Carlos Jesus Pereira Haygert, Lilian Gerdi Kittel Ries, and Eliane Castilhos Rodrigues Corrêa. “Diaphragmatic amplitude and accessory inspiratory muscle activity in nasal and mouth-breathing adults: a cross-sectional study.” Journal of Electromyography and Kinesiology 25, no. 3 (2015): 463-468.
57Deacon, Naomi L., Rachel Jen, Yanru Li, and Atul Malhotra. “Treatment of obstructive sleep apnea. Prospects for personalized combined modality therapy.” Annals of the American Thoracic Society 13, no. 1 (2016): 101-108.
58Huang YS, Quo S, Berkowski JA, Guilleminault C (2015) Short Lingual Frenulum and Obstructive Sleep Apnea in Children. Int J Pediatr Res 1:003
By Jan 04, 2026
By Oct 12, 2025
By Oct 01, 2025
By Aug 10, 2025
By Jul 10, 2025
By Jul 05, 2025