Child Mouth Breathing Therapy – Support for Sleep, Focus, and Facial Development
Is your child always breathing through their mouth, even at rest or during sleep? Mouth breathing can affect growth, energy, and focus—but we can help retrain the root cause.
"In children, the harmful effects of mouth breathing are serious. During these formative years, the breathing helps to shape the face, teeth and airways.
Nasal breathing, with the tongue in its correct resting position, contributes to healthy growth.
Oral breathing contributes to irregular growth and poor development. Because it causes poor brain oxygenation, mouth breathing has also been linked with poor cognitive development and behavioral disorders including attention deficit hyperactivity disorder (ADHD)."27
1
Nose Breather
Better Brain Function2
Better Memory & Information Retention2
More Focused2
Helps Relax. Reducing stress by lowering the harmful effects of cortisol in the body3
Better Brain Development in Kids27,28
More Attractive Features4
Prevents Long Face Syndrome4
Nicely Defined Cheekbones4
Well Developed Jawline4
Straighter Teeth4
Better Formed Upper Airways4
Brighter Alert Eyes4
Improved Posture5
Enhanced Core Muscle Stability6
Healthier
Adequate Saliva & Fresher Breath. Less Cavities & Gum Disease7
Growth Hormone Release is Important During a Child's Growing Years and Builds, Maintains, & Repairs Tissues9
Can Help Prevent Snoring & Apnea Episodes7
Helps Prevent ADHD18,27
Better Rested7
Nitric Oxide Intake (Only Created in the Nose)10
Immune Defense: Combats Harmful Bacteria, Viruses, & Parasitic Organisms11
Regulates Blood Pressure: is a Vasodilator11
Enhances the Lungs Capacity to Absorb Oxygen11
Maintaining Homeostasis in the Body: pH, Temperature, Ion, & Glucose Concentration12
Neurotransmission12
Mouth Breather
Brain Fog14
Decreased Productivity13
Poorer Academics: Performing Poorly at School14
Poorer Quality of Life15
Increased Stress8
Less Attractive Features
Poorly Defined Cheekbones16
Narrow Jaw & Face16
Jaw Set Back16
Crooked/Crowded Teeth16
Gummy Smile16
Tired Eyes: Dark Circles & Unfocused16
Underdeveloped Nasal Airway16
Smaller Airway16
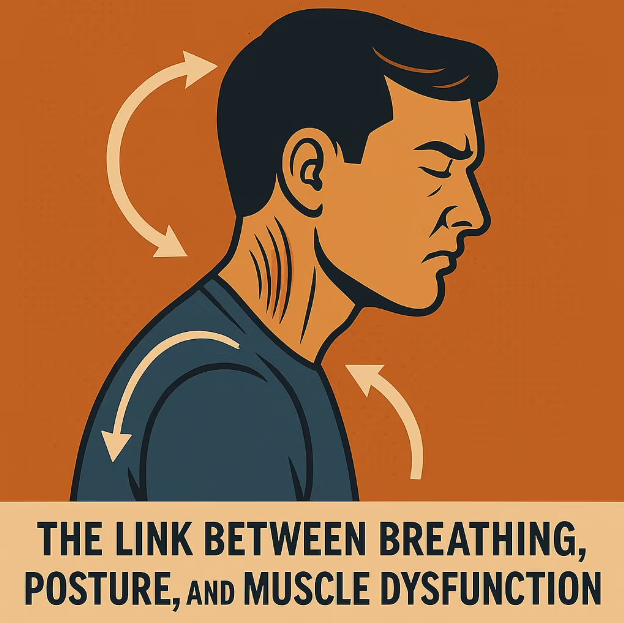
Postural Problems: Forward Head Posture17
Muscle Fatigue17
Neck Pain17
Jaw Tension17
Spinal Disc Compression17
Early Arthritis17
Tension Headaches17
Dental Occlusal Problems17
Decreasing Health
Sleep Apnea: Breathing Stops While Asleep for a Varying Length of Time20
ADHD18,27
Depression21
Reduced Growth Hormone Production19
Dry Mouth, Sore Throat, Headaches, Trouble Paying Attention, & Irritability20
Weakened Immune System: Reduced Number of T-Cells20
Memory Loss: Sleep Helps to Consolidate Memories20
Mental Confusion20
Tired13
Fatigue20
High Blood Sugar Levels23
Deprives Body of Needed Oxygen Levels20
Acid Reflux20
Asthma25
High Blood Pressure: Drops in Blood Oxygen Levels Strains the Cardiovascular System20
Minimal to No Nitric Oxide Intake Can Cause (In Their Later Years)10
High Blood Pressure10
Heart Disease10
Heart Attack10
Stroke10
Digestive Track Issues10
Alzheimer's Disease10
Dementia10
Bladder Issues10
Snoring18
Abnormal Cholesterol: May have Higher LDL22
Linked to Fatty Liver Disease24
Apnea18
What is Orofacial Myofunctional Therapy Capable Of?
At Oral-Facial Advantage, we guide your child's growth towards a more balanced oral-facial foundation. Aiding to prevent, or soothe the many disorders you see through-out this website.
Reflexive vs. Conscious
We chew, swallow, breathe, and rest our mouths as an un-trained reflexive habit.
The Oral-Facial Advantage Program is a personalized straightforward set of exercises, scientifically designed to build new beneficial long-term muscle-memories.
At What Age Can My Child Begin Oral-Facial Muscle Therapy?
The younger the child the more flexible their physiology, and behavior.
Mature 3 to 4 year old mouth breathers can learn nasal breathing.
Mentally prepared 5 year old's can begin the Oral Habit Elimination Program.
7 to 8+ year old's can start their Oral-Facial Advantage Program.
Who is Eligible for a Free Consult?
Everyone.
All ages can come in for a free consult.
It is a great opportunity for your questions to be answered, and for the Orofacial Myologist to assess your child's readiness for the program.
Book a Free In-Person Consultation Today
What is Orofacial Myofunctional Therapy?
The mouth, head, and neck are a complex weave of muscles, tissues, joints, bones, blood vessels, and nerves that all need to work together for a smooth, discomfort free daily function.
Currently, we are born and grow with little direction and training in this area of our bodies. We eat the way we eat, we chew on the side that is most comfortable, we swallow whichever way gets the food down, our tongues rest wherever they rest, we breathe the easier way, and we have repetitive habits that soothe our stress that can involve our faces and mouths.
All of these reflexive habits can create abnormalities in your child's oral and facial structures, and since they have been doing them throughout their youthful growth, their bones and muscles have molded around these untrained habits, potentially creating ingrained disorders in their later years.
Orofacial Myofunctional Therapists specialize and only focus on the muscles and tissues throughout the tongue, jaw, face, head, and neck. Weekly exercises are given that either tone or relax these muscles and tissues aligning them to your child's center. Working from their foundation up. Progressively resetting years of habits. Most children will complete the program within the year and yet their new symmetry could last their lifetime.
A Stanford University Systematic Review revealed the lasting beneficial effects of Orofacial Myofunctional Therapy in a wide cohort:
“Current literature demonstrates that orofacial myofunctional therapy decreases apnea-hypopnea index by approximately 50% in adults and 62% in children. Improvements to snoring and daytime sleepiness. Shown effective in children and adults of all ages studied thus far; youngest patient 3 yrs old to 60 yrs old. Therapy has an important role in preventing relapse.”48
1Breathe Institute Image
2Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics and behaviour. General dentist. 2010 Jan- Feb; 58 (1): 18-25.
2Surtel A, Klepacz R, Wysokińska-Miszczuk J. Wpływ toru oddechowego na jamę ustną. The influence of breathing mode on the oral cavity. Pol Merkur Lekarski. 2015 Dec;39(234):405-7. Polish. PMID: 26802697.
3Steffen, Patrick R et al. “The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood.” Frontiers in public health vol. 5 222. 25 Aug. 2017, doi:10.3389/fpubh.2017.00222
4Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics and behaviour. General dentist. 2010 Jan- Feb; 58 (1): 18-25.
4Pereira F, Motonaga S, Faria P, Matsumoto M, Trawitzki L, Lima S, Lima W. Myofunctional and Cephalometric Evaluation of Mouth Breathers. Brazilian Journal of Otorhinolaryngology. 2001. 67 (1): 43-49.
4Surtel A, Klepacz R, Wysokińska-Miszczuk J. Wpływ toru oddechowego na jamę ustną. The influence of breathing mode on the oral cavity. Pol Merkur Lekarski. 2015 Dec;39(234):405-7. Polish. PMID: 26802697.
5Paskay L. OMD Orofacial Myofunctional Disorders: Assessment, prevention and treatment. JAOS. 2012 march-april; 34-40.
5Okuro RT, Morcillo AM, Ribeiro MÂ, Sakano E, Conti PB, Ribeiro JD. Mouth breathing and forward head posture: effects on respiratory biomechanics and exercise capacity in children. J Bras Pneumol.2011 Jul-Aug; 37(4):471-9.
5Damaging Effects of Forward Head Posture.(2015, January 22). Retrieved from http://www.denvertechchiro.com/files/fhp_revised.pdf
6Tomonori Iwasaki, Issei Saitoh, Yoshihiko Takemoto. Tongue posture improvement and pharyngeal airway enlargement as secondary effects of rapid maxillary expansion: A cone-beam computed tomography study. AJO-DO Volume 143, Issue 2, P235-245, Feb 01 2013.
6Key, Josephine. “‘The core’: understanding it, and retraining its dysfunction.” Journal of bodywork and movement therapies 17, no. 4 (2013): 541-559.
7Surtel A, Klepacz R, Wysokińska-Miszczuk J. Wpływ toru oddechowego na jamę ustną. The influence of breathing mode on the oral cavity. Pol Merkur Lekarski. 2015 Dec;39(234):405-7. Polish. PMID: 26802697.
8Steffen, Patrick R et al. “The Impact of Resonance Frequency Breathing on Measures of Heart Rate Variability, Blood Pressure, and Mood.” Frontiers in public health vol. 5 222. 25 Aug. 2017, doi:10.3389/fpubh.2017.00222
9Davidson, J R et al. “Growth hormone and cortisol secretion in relation to sleep and wakefulness.” Journal of psychiatry & neuroscience : JPN vol. 16,2 (1991): 96-102.
9Takahashi, Y et al. “Growth hormone secretion during sleep.” The Journal of clinical investigation vol. 47,9 (1968): 2079-90. doi:10.1172/JCI105893
9Honda, Y et al. “Growth hormone secretion during nocturnal sleep in normal subjects.” The Journal of clinical endocrinology and metabolism vol. 29,1 (1969): 20-9. doi:10.1210/jcem-29-1-20
10Djupesland PG, Chatkin JM, Qian W, Haight JS. Nitric oxide in the nasal airway: a new dimension in otorhinolaryngology. Am J Otolaryngol.2001 Jan; 22(1): 19-32.
11Lundberg J, Weitzberg E. Nasal nitric oxide in man. Thorax.1999;(54):947-952
12Chang H R. Nitric Oxide, the Mighty Molecule: Its Benefits for Your Health and Well-Being. 1st ed. United States. ; 2011
13Lunn M, Craig T. Rhinitis and sleep. Sleep Med Rev. 2011 Oct;15(5):293-9
13Muliol J, Maurer M, Bousquet J. Sleep and allergic rhinitis. Journal Investigation Allergol Clinical Immunology. 2008;18(6):415-9.
13Ohki M, Usui N, Kanazawa H, Hara I, Kawano K. Relationship between oral breathing and nasal obstruction in patients with obstructive sleep apnoea. Acta Otolaryngol Suppl. 1996;523:228-30.
13Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics and behaviour. General dentist. 2010 Jan- Feb; 58 (1): 18-25.
13Surtel A, Klepacz R, Wysokińska-Miszczuk J. Wpływ toru oddechowego na jamę ustną. The influence of breathing mode on the oral cavity. Pol Merkur Lekarski. 2015 Dec;39(234):405-7. Polish. PMID: 26802697.
14Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics and behaviour. General dentist. 2010 Jan- Feb; 58 (1): 18-25.
15Lunn M, Craig T. Rhinitis and sleep. Sleep Med Rev. 2011 Oct;15(5):293-9
15Muliol J, Maurer M, Bousquet J. Sleep and allergic rhinitis. Journal Investigation Allergol Clinical Immunology. 2008;18(6):415-9.
15Ohki M, Usui N, Kanazawa H, Hara I, Kawano K. Relationship between oral breathing and nasal obstruction in patients with obstructive sleep apnoea. Acta Otolaryngol Suppl. 1996;523:228-30.
16Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics and behaviour. General dentist. 2010 Jan- Feb; 58 (1): 18-25.
16Pereira F, Motonaga S, Faria P, Matsumoto M, Trawitzki L, Lima S, Lima W. Myofunctional and Cephalometric Evaluation of Mouth Breathers. Brazilian Journal of Otorhinolaryngology. 2001. 67 (1): 43-49.
16Paskay L. OMD Orofacial Myofunctional Disorders: Assessment, prevention and treatment. JAOS. 2012 march-april; 34-40.
16Surtel A, Klepacz R, Wysokińska-Miszczuk J. Wpływ toru oddechowego na jamę ustną. The influence of breathing mode on the oral cavity. Pol Merkur Lekarski. 2015 Dec;39(234):405-7. Polish. PMID: 26802697.
16Okuro RT, Morcillo AM, Ribeiro MÂ, Sakano E, Conti PB, Ribeiro JD. Mouth breathing and forward head posture: effects on respiratory biomechanics and exercise capacity in children. J Bras Pneumol.2011 Jul-Aug; 37(4):471-9.
17Okuro RT, Morcillo AM, Ribeiro MÂ, Sakano E, Conti PB, Ribeiro JD. Mouth breathing and forward head posture: effects on respiratory biomechanics and exercise capacity in children. J Bras Pneumol.2011 Jul-Aug; 37(4):471-9.
17Damaging Effects of Forward Head Posture.(2015, January 22). Retrieved from http://www.denvertechchiro.com/files/fhp_revised.pdf
18Lunn M, Craig T. Rhinitis and sleep. Sleep Med Rev. 2011 Oct;15(5):293-9
18Muliol J, Maurer M, Bousquet J. Sleep and allergic rhinitis. Journal Investigation Allergol Clinical Immunology. 2008;18(6):415-9.
18Ohki M, Usui N, Kanazawa H, Hara I, Kawano K. Relationship between oral breathing and nasal obstruction in patients with obstructive sleep apnoea. Acta Otolaryngol Suppl. 1996;523:228-30.
18Jefferson Y. Mouth breathing: adverse effects on facial growth, health, academics and behaviour. General dentist. 2010 Jan- Feb; 58 (1): 18-25.
18Surtel A, Klepacz R, Wysokińska-Miszczuk J. Wpływ toru oddechowego na jamę ustną. The influence of breathing mode on the oral cavity. Pol Merkur Lekarski. 2015 Dec;39(234):405-7. Polish. PMID: 26802697.
18Fitzpatrick MF, McLean H, Urton AM, Tan A, O’Donnell D, Driver HS. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J. 2003 Nov;22(5):827-32.
18“ADHD and Sleep.” ADHD & Sleep Problems-National Sleep Foundation. National Sleep Foundation, 2017. Web. 11 Feb.2017. https://sleepfoundation.org/sleep-disorders-problems/adhd-and-sleep.
18Shur-Fen Gau S. Prevalence of sleep problems and their association with inattention/hyperactivity among children aged 6-15 in Taiwan.J Sleep Res. 2006 Dec;15(4):403-14.
18Borres MP. Allergic rhinitis: more than just a stuffy nose. Acta Paediatrica. 2009 Jul;98(7):1088-92)
19Davidson, J R et al. “Growth hormone and cortisol secretion in relation to sleep and wakefulness.” Journal of psychiatry & neuroscience : JPN vol. 16,2 (1991): 96-102.
19Takahashi, Y et al. “Growth hormone secretion during sleep.” The Journal of clinical investigation vol. 47,9 (1968): 2079-90. doi:10.1172/JCI105893
19Honda, Y et al. “Growth hormone secretion during nocturnal sleep in normal subjects.” The Journal of clinical endocrinology and metabolism vol. 29,1 (1969): 20-9. doi:10.1210/jcem-29-1-20
20Fitzpatrick MF, McLean H, Urton AM, Tan A, O’Donnell D, Driver HS. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J. 2003 Nov;22(5):827-32.
21Ejaz, Shakir M et al. “Obstructive sleep apnea and depression: a review.” Innovations in clinical neuroscience vol. 8,8 (2011): 17-25.
22Gunduz C, et al "Obstructive sleep apnea independently predicts lipid levels: Data from the European Sleep Apnea Database" Respirology 2018; DOI: 10.1111/resp.13372.
23Jimmy Doumit, Bharati Prasad. "Sleep Apnea in Type 2 Diabetes" Diabetes Spectrum 2016 Feb; 29(1): 14-19.
24Omar A. Mesarwi, Rohit Loomba, Aul Malhotra. "Obstructive Sleep Apnea, Hypoxia, and Nonalcoholic Fatty Liver Disease" ATS Journals 2018 Nov; V199, I7.
25Bharati Prasad, Sharmilee M. Nyenhuis, Ikuyo Imayama. "Asthma and Obstructive Sleep Apnea Overlap: What has the evidence taught us?" ATS Journals 2019 Dec;V201, I11.
26Camacho, Macario et al. “Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review and Meta-analysis.” Sleep vol. 38,5 669-75. 1 May. 2015, doi:10.5665/sleep.4652
By Jan 04, 2026
By Oct 12, 2025
By Oct 01, 2025
By Aug 10, 2025
By Jul 10, 2025
By Jul 05, 2025