Tongue-Tie Release Isn’t Enough: Post-Frenectomy Exercises Every Ottawa Parent Should Know (2025 update)
Pre- and Post-Frenectomy Therapy Every Ottawa Parent Should Know (2025 Update)
Key takeaway: A simple clip isn’t the cure. Without therapy, the tongue may stay “lazy” or reattach. Pre- and post-frenectomy myofunctional therapy promotes full mobility, supports healthy speech and breathing, and helps prevent relapse.
“The release of a lingual frenulum without functional re-education of the tongue may be insufficient in resolving orofacial dysfunction.”
— Harvard Medical School, Journal of Clinical Pediatric Dentistry, 2023
Why Before-and-After Care Matters
| Fact | What It Means for Your Child |
|---|---|
| 5–13% of tongue-tie releases need a second surgery when no therapy is done. (Dr. Oracle) | Scar tissue can pull the tongue back down. |
| Revision rates drop below 1% when families follow a simple therapy plan. (ScienceDirect, 2025) | Gentle movement helps the wound heal soft, not tight. |
| Therapy before release improves surgical outcomes by retraining tongue function in advance. | Your child gains tongue awareness before the procedure, so they recover faster and adapt better. |
Bottom line: A frenectomy frees the tongue—but therapy teaches it how to move.
What Can Go Wrong Without Preparation

Scar tethering
Tongue edges blanch or curl when lifted; restricted motion returns.
Oral-motor habits
Lip-biting, mouth breathing, or incorrect swallowing patterns persist.
Infants
For children under 2, please speak with a lactation consultant before proceeding with any therapy or release.
Speech delays
Trouble with sounds like “l,” “r,” or “s”; ongoing articulation concerns past age 4.
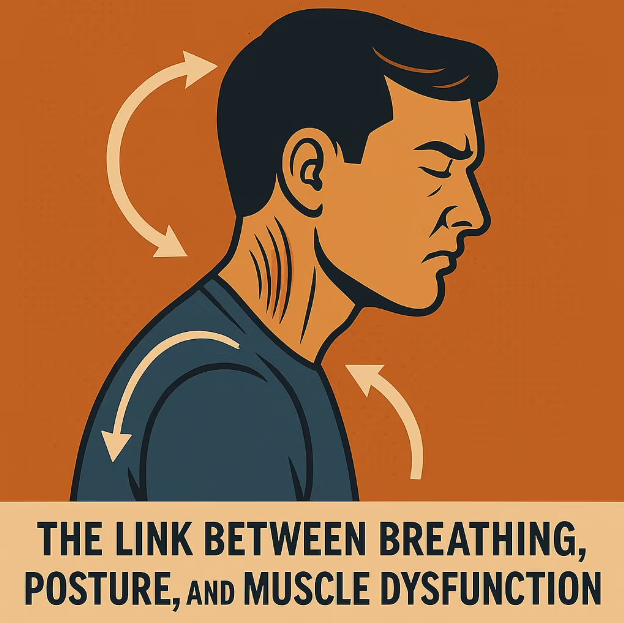
Open-mouth breathing
Dry lips, noisy sleep, tongue low and forward.
Dental & Orthodontic issues
Shifting teeth, open bite, or relapse after braces and aligners.
Our “Prep → Release → Retrain” Framework

1. Prep Phase
Before the procedure, we focus on gentle exercises that improve tongue mobility, coordination, and awareness.
This helps the muscles and nervous system adapt so that once the tissue is released, the tongue is ready to move freely and effectively.

2. Release Support
During the release, we work closely with your chosen provider to ensure the procedure is smooth and well-supported.
We guide you through wound care, provide healing strategies, and give you a clear aftercare plan so recovery is as comfortable as possible.

3. Retrain Phase
After the initial healing, therapy shifts to building lasting function.
We retrain the tongue and surrounding muscles for strength, balance, and proper coordination—helping to restore natural swallowing, breathing, and speaking patterns.

4. Long-Term Success
Lasting results come from more than just the release itself. Therapy before, during, and after ensures the tongue gains strength, flexibility, and coordination.
This full approach is what leads to stable, life-changing improvements.
Signs Your Child Might Need Support
☑ Tongue mobility is limited — heart-shaped tip, difficulty lifting to the roof of the mouth, or not extending past the lips
☑ Speech isn’t improving — progress feels stuck, words sound unclear, or therapy isn’t moving forward
☑ Breathing concerns — mouth breathing, open-mouth posture, or snoring that continues after the release
☑ Eating struggles — gagging, picky chewing patterns, or tongue-thrust swallowing
☑ Oral habits persist — thumb sucking, pacifier use, or lip biting that doesn’t fade on its own
☑ Facial or jaw strain — frequent tension, headaches, or discomfort around the mouth, jaw, and/or neck
1. UHS NHS. Frenulotomy (Tongue-Tie Release) Exercises – Patient Factsheet (UHS NHS)
2. Scoping Review: Outcomes of Stretching Exercises After Lingual Frenotomy in Infants (2025) (ScienceDirect)
3. MDPI. Pre- and Post-Operative Care Protocol for Tongue-Tie in Children (2024)
4. Dr. Oracle AI Summary. Lingual Frenectomy Re-Attachment Rates (5–13%) (2025)
Updated May 21, 2025 — reviewed annually for new research and local best practices.
How Orofacial Myofunctional Therapy Helps
Every patient starts with a complete 90–120 minute assessment at our Ottawa clinic. From there, we guide you step by step with a mix of personalized exercises, monitoring, and collaboration to ensure lasting results.
| Steps | What You Get |
|---|---|
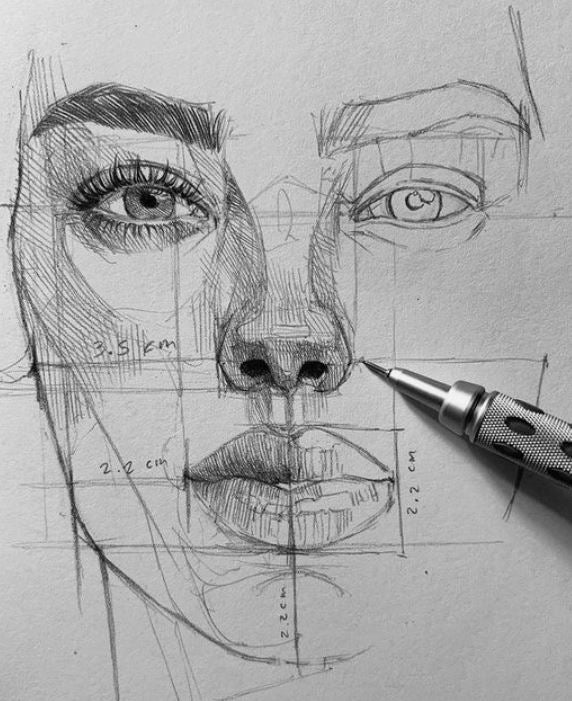
| Assessment & Exam | Photos, videos, and a detailed assessment to understand your breathing, posture, and tongue function. We set clear goals before therapy begins. |
| Coaching | One-on-one sessions with personalized exercises, practical guidance, and ongoing encouragement to keep progress steady. |
| Progress Monitoring | We take regular measurements to track your progress, fine-tune your plan, and celebrate wins along the way. This ensures steady improvement and helps prevent setbacks. |
| Team Collaboration | We coordinate with your ENT, dentist, or speech therapist when needed, making sure everyone is on the same page for your care. |
Assessment
Airway screening, muscle tone tests, photos & measurements.
Personalized exercises
One-on-one coaching and exercise plan.
Habit reinforcement
Bi-weekly check‑ins, daytime and sleep‑time strategies.
Take home message
Frenectomy is just one piece of the puzzle. Real results come from retraining the tongue’s movement—before and after surgery. With support, your child can chew, speak, and breathe better for life.